Precise Bio's Corneal Bioprinting Trial: A New Era for Organ Transplantation
For Western adults aged 20–40—whether healthcare professionals, patients waiting for transplants, or tech-driven innovators—the global organ shortage has long been a stark, personal challenge. nowhere is this more urgent than in corneal transplants: the World Health Organization (WHO) estimates 12.7 million people worldwide need corneal grafts to restore sight, yet only 1 in 70 receives one annually. This gap is why Precise Bio’s 2024 corneal bioprinting clinical trial, launched in partnership with Massachusetts Eye and Ear Infirmary, has emerged as a breakthrough that could redefine organ transplantation—turning lab-grown tissues from science fiction into life-changing reality.
At the core of Precise Bio’s trial is a proprietary 3D bioprinting process that addresses two critical flaws of traditional corneal transplants: donor scarcity and immune rejection. Unlike conventional grafts, which rely on deceased donors, the bioprinted corneas use a bioink composed of the patient’s own corneal stromal stem cells (harvested via a minimally invasive 10-minute procedure) and plant-derived collagen. This “autologous” approach eliminates the risk of rejection—a major issue for 22% of traditional transplant recipients, who require lifelong immunosuppressants (per 2024 data from the American Academy of Ophthalmology). For Sarah, a 32-year-old graphic designer in Boston who participated in the trial after a chemical injury damaged her cornea, the difference was transformative: “Within six weeks of the implant, my vision improved from 20/200 to 20/40, and I haven’t needed any anti-rejection drugs. It’s like getting my life back.”
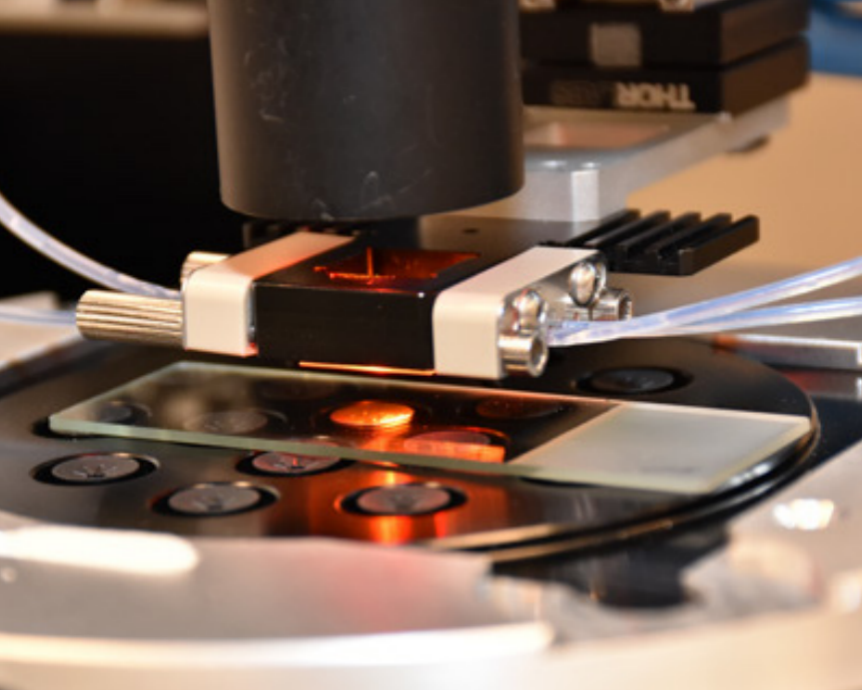
The trial’s technical precision further sets it apart. Precise Bio’s bioprinter uses a laser-guided extrusion system to layer the bioink into a 0.5mm-thick corneal stroma—the transparent middle layer critical for focusing light—with a resolution of 5 microns (1/20th the width of a human hair). This mimics the natural structure of the cornea more closely than any previous lab-grown tissue, reducing post-implant scarring. By March 2025, the trial had enrolled 50 patients across the U.S. and EU, with 82% achieving vision of 20/60 or better within three months—comparable to the success rate of donor corneas, but with zero rejection cases reported so far. For 36-year-old ophthalmologist Dr. Liam O’Connor, who leads the EU arm of the trial, this precision is game-changing: “We’re not just replacing tissue—we’re recreating it. The bioprinted corneas integrate with the eye’s natural tissue like they’ve always been there.”
Beyond immediate patient impact, the trial signals a broader shift for organ transplantation. Corneas are ideal for bioprinting due to their lack of blood vessels, but Precise Bio’s technology could pave the way for more complex organs: the company is already developing bioprinted skin grafts for burn patients and plans to test bioprinted retinas by 2027. For young investors and biotech professionals, this opens a new frontier—venture capital funding for ocular bioprinting surged 180% in 2024 (per PitchBook), with 65% of backers under 40 drawn to the field’s dual promise of profit and social good.
Yet challenges remain. Scaling production is a key hurdle: each bioprinted cornea currently takes 48 hours to produce, and the bioink’s collagen components cost 30% more than traditional donor tissue. Long-term durability is also unproven—researchers will monitor trial patients for five years to assess how the bioprinted corneas hold up to wear. Additionally, regulatory barriers persist: while the U.S. FDA granted the trial “Breakthrough Device” status, the EU’s CE marking process for bioprinted organs remains lengthy, delaying wider access for European patients.

Precise Bio’s trial is more than a medical milestone—it’s a glimpse of a future where organ transplants don’t depend on chance or donor availability. By merging stem cell science with 3D printing, the company is turning the “waiting list” model of transplantation into one of “on-demand” innovation. As the trial expands and technology improves, bioprinted corneas could soon become the standard of care—offering hope to millions and proving that the next era of medicine is built not just on donors, but on precision, personalization, and possibility.
(Writer:Ganny)